What is this specialized procedure for treating arterial blockages? A novel approach to vascular intervention.
This minimally invasive technique utilizes a specialized catheter and cutting mechanism to remove plaque buildup within blood vessels. It targets specific areas of blockage in arteries, particularly those leading to the heart or brain. The procedure involves delicate manipulation of tools within the circulatory system, offering a targeted and controlled approach to address the buildup. Often used in cases where traditional methods prove less effective, this technique offers a potential solution for patients with narrowed or obstructed arteries. A critical component is the accurate and precise delivery of the device to the blockage site.
The benefits of this procedure often lie in its precision and reduced invasiveness compared to other options. Minimizing tissue damage and recovery time is a key aspect. The goal is to restore optimal blood flow, thereby alleviating symptoms and potentially preventing further complications like heart attack or stroke. The procedure's efficacy depends heavily on the skill and expertise of the medical team executing it and patient factors. A detailed assessment of the patient's vascular system is essential beforehand.
Moving forward, the discussion will explore the specific applications of this type of intervention within the context of atherectomy. This will involve analyzing case studies, evaluating its safety profile, and comparing it to other similar treatment methods.
Hawkone Atherectomy
Understanding the key aspects of hawkone atherectomy is crucial for assessing its role in vascular interventions. Precise application, minimal invasiveness, and patient-specific factors are fundamental.
- Minimally invasive approach
- Targeted plaque removal
- Specialized catheter design
- Controlled tissue manipulation
- Improved blood flow restoration
- Reduced recovery time
- Surgical precision
These key aspects highlight the intricate nature of hawkone atherectomy. Minimally invasive procedures, such as this, are favored for their reduced recovery times and potential for faster patient rehabilitation. Targeted plaque removal is a vital component, impacting blood flow restoration to affected regions. Specialized catheter design ensures precise delivery and control, while controlled tissue manipulation minimizes collateral damage. The importance of surgical precision and meticulous patient assessment cannot be overstated. Successful outcomes rely on a blend of advanced technology, skilled professionals, and patient-specific factors, ultimately contributing to improved long-term vascular health.
1. Minimally Invasive Approach
The "minimally invasive approach" is a defining characteristic of hawkone atherectomy. This approach centers on the use of specialized instruments and techniques to target and remove plaque buildup within blood vessels with minimal disruption to surrounding tissues. The goal is to achieve comparable therapeutic outcomes to more extensive procedures while minimizing trauma, recovery time, and potential complications. This approach is crucial for the success of hawkone atherectomy, as it enables precise targeting of affected arterial segments, potentially reducing the risk of adverse events associated with larger incisions or more extensive surgical interventions.
This focus on minimizing invasiveness translates into several practical advantages. Reduced tissue trauma leads to shorter hospital stays and faster patient recovery. Minimized blood loss during the procedure is a further benefit, impacting patient safety. The emphasis on minimally invasive techniques is also associated with a lower incidence of post-operative complications, such as infection or bleeding. Furthermore, patients frequently experience faster return to normal activities and an improved quality of life. Real-world examples can be seen in the increasing adoption of minimally invasive surgical procedures across various specialties, demonstrating the widespread value of this approach in healthcare. The impact is readily apparent in patient satisfaction, reduced healthcare costs, and improved surgical outcomes.
In summary, the minimally invasive approach is intrinsically linked to the efficacy and safety of hawkone atherectomy. This approach underscores a crucial shift towards less invasive therapies, offering significant advantages for both patients and healthcare systems. While challenges like precise device delivery and procedural mastery may still exist, the benefits of minimizing invasiveness in this specialized vascular intervention remain paramount. The long-term implications for patient care and treatment options are substantial.
2. Targeted Plaque Removal
Targeted plaque removal is a critical component of hawkone atherectomy. This precision-based approach is designed to address specific areas of arterial blockage without unnecessary damage to surrounding healthy tissue. Its efficacy hinges on the ability to precisely identify and isolate problematic plaque deposits while minimizing collateral damage.
- Precision and Minimization of Damage
Hawkone atherectomy relies on a highly specialized catheter and cutting mechanism. This design allows for controlled removal of plaque within the affected artery. This targeted approach contrasts with more general methods, aiming for less tissue trauma and faster recovery times. Careful selection of the precise location of the intervention is crucial for avoiding damage to the vessel walls and other critical structures.
- Restoration of Blood Flow
Effective plaque removal is paramount in restoring healthy blood flow. By directly addressing the obstruction caused by plaque buildup, targeted methods like hawkone atherectomy can alleviate symptoms associated with narrowed or blocked arteries. This improvement in blood flow helps prevent further complications such as heart attack or stroke, potentially improving the patient's overall cardiovascular health and reducing the risk of adverse events.
- Improved Treatment Outcomes
The targeted nature of plaque removal within hawkone atherectomy contributes to enhanced treatment outcomes. Specific plaque areas are addressed, enabling a more effective restoration of normal blood flow compared to less focused procedures. The outcome directly correlates with the successful removal of obstructing material and the preservation of healthy tissue. This specificity allows for a higher likelihood of positive outcomes and a reduced risk of complications.
- Minimizing Systemic Impact
Focusing on a localized area, hawkone atherectomy is designed to minimize the overall impact on the patient's body. By precisely removing plaque, the procedure avoids the potential side effects and systemic disturbances that may arise from more widespread interventions. This reduced systemic impact leads to potentially more manageable post-operative recovery periods and a better overall patient experience.
In conclusion, the targeted nature of plaque removal in hawkone atherectomy is a key factor in maximizing efficacy and minimizing potential complications. This precision-driven approach directly addresses the blockage, restoring blood flow and potentially improving long-term cardiovascular health. By focusing on the specific problem areas, the procedure stands out compared to other methods.
3. Specialized Catheter Design
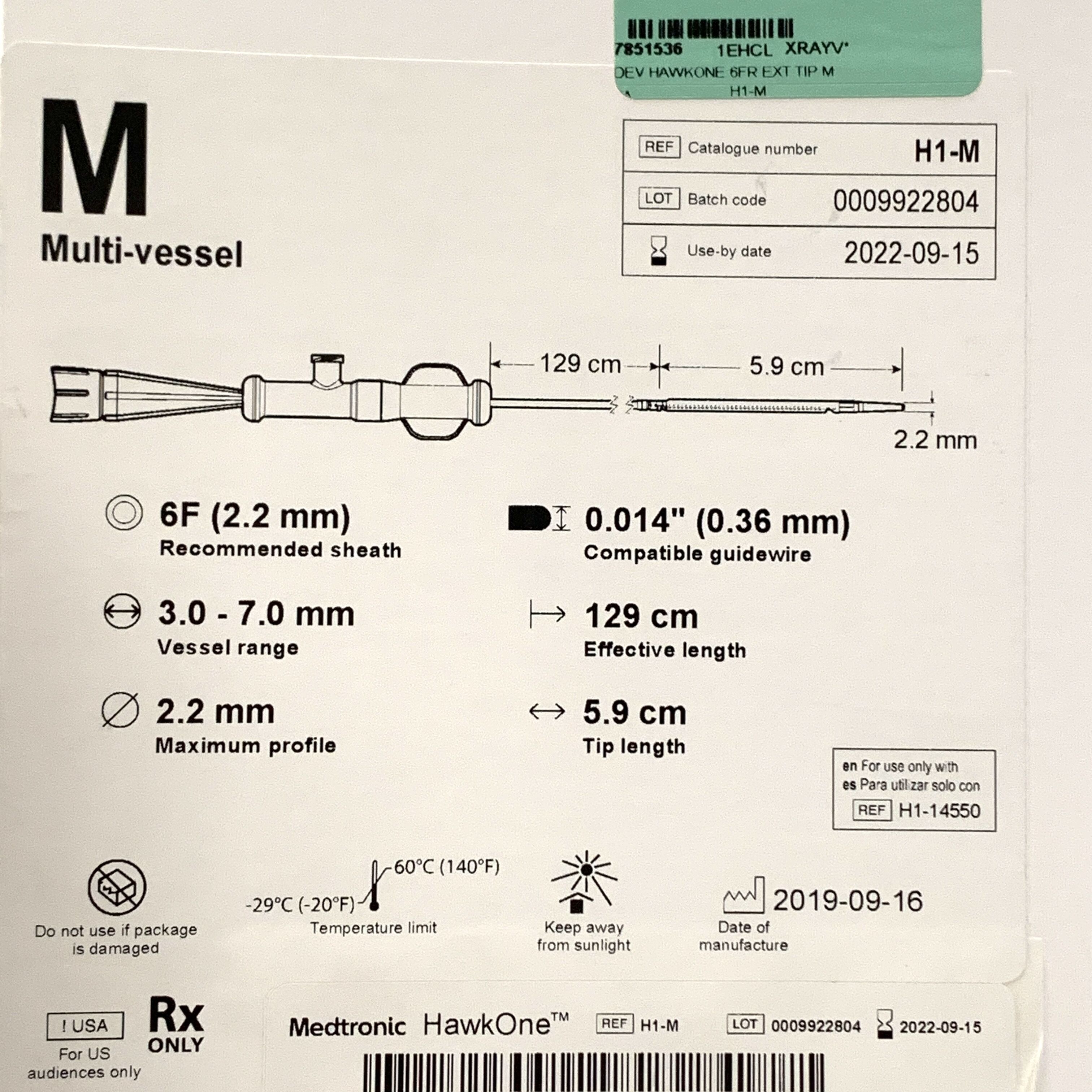
The effectiveness of hawkone atherectomy is intrinsically linked to the design of the specialized catheter. This specialized instrument plays a pivotal role in the precision and safety of the procedure, enabling targeted plaque removal and minimizing collateral damage.
- Angiographic Guidance and Navigation
Specialized catheters in this procedure often incorporate advanced imaging capabilities. These systems allow real-time visualization of the targeted artery, enabling precise positioning and maneuvering of the catheter to the precise location of the blockage. This feature facilitates accurate delivery of the atherectomy device, minimizing the risk of unintended damage to healthy tissue. The integration of imaging technology within the catheter is crucial for navigating intricate vascular pathways and facilitating precise targeting of the plaque deposits.
- Controlled Cutting Mechanism
The catheter's design often features an integrated cutting mechanism. This mechanism is crucial for effectively removing plaque while preserving the integrity of the vessel wall. The design dictates the precision and control exerted during plaque removal. The catheter's cutting mechanism must be designed to minimize vessel trauma, ensuring the safety and efficacy of the procedure. The controlled nature of the cutting action limits the damage to the surrounding vascular structures and enables a targeted approach to plaque removal.
- Minimally Invasive Access and Delivery
The catheter's design facilitates minimally invasive access to the target area. This characteristic minimizes the extent of the procedure, contributing to a reduced recovery time. The small size of the catheter and the precise placement mechanisms minimize tissue trauma, enabling a more efficient approach. This aspect is vital for patient comfort and well-being, reducing the risk of complications and promoting faster healing.
- Optimized Plaque Retrieval System
Some designs incorporate mechanisms to effectively capture and remove the fragmented plaque from the vascular system. These optimized retrieval systems ensure that the removed plaque material is effectively captured and removed, minimizing the risk of emboli formation. The design of the catheter impacts the efficiency of this process, thereby affecting the potential for complications. Preventing emboli is paramount in maintaining optimal blood flow and minimizing the risk of downstream complications.
In conclusion, the specialized catheter design in hawkone atherectomy is paramount. By integrating precise navigation, controlled cutting mechanisms, minimally invasive access, and effective plaque retrieval, the procedure can optimize outcomes while minimizing invasiveness. This sophisticated design directly contributes to the safety, efficiency, and effectiveness of the overall procedure.
4. Controlled Tissue Manipulation
Controlled tissue manipulation is a critical component of hawkone atherectomy. The procedure hinges on the ability to precisely and selectively remove plaque deposits within blood vessels without causing undue damage to surrounding healthy tissue. This necessitates sophisticated instrumentation and meticulous procedural execution. The intricate nature of the vascular system demands precise maneuvering to minimize injury to delicate structures and maintain the integrity of the arterial walls. Failure to achieve controlled manipulation could lead to complications like vessel perforation, embolus formation, or unintended damage to surrounding nerves or tissues. The degree of control directly influences the procedure's safety profile and potential for achieving optimal outcomes.
Real-world examples of the importance of controlled tissue manipulation in similar atherectomy procedures demonstrate its significance. Careful, controlled manipulation reduces the risk of post-procedural complications. Studies have shown that the rate of complications is significantly lower in cases where procedural steps exhibit a high degree of precision and control. This translates into improved patient outcomes and shorter recovery periods. Effective control during plaque removal contributes to the restoration of normal blood flow without causing further harm, minimizing the likelihood of vessel spasms or inflammatory responses. Minimizing damage also contributes to the long-term structural integrity of the vessel and the overall health of the circulatory system. Clinical experience further underscores the vital role of precisely controlled tissue manipulation in ensuring successful and safe atherectomy procedures.
In conclusion, controlled tissue manipulation is not merely a technical aspect of hawkone atherectomy but a fundamental prerequisite for achieving optimal patient outcomes. Its significance stems from the delicate nature of the vascular system and the need to minimize unintended damage. The degree of control exerted during the procedure directly influences the safety profile and long-term success of the intervention. Understanding and applying these principles of controlled manipulation are crucial for reducing complications and improving patient care in vascular interventions. Maintaining precise control over the instruments and the procedure is essential for minimizing risks and maximizing positive outcomes. This approach prioritizes the delicate balance between effective treatment and minimizing potential harm.
5. Improved blood flow restoration
Improved blood flow restoration is a crucial objective in hawkone atherectomy. The procedure's core function is to address arterial blockages caused by plaque buildup, thereby enhancing blood flow to the affected areas. This restoration is vital for preventing further complications and maintaining optimal cardiovascular health. Understanding the mechanisms and implications of this restoration is critical in evaluating the efficacy of the intervention.
- Reduced Symptoms and Improved Quality of Life
Enhanced blood flow directly alleviates symptoms stemming from reduced perfusion, such as chest pain (angina) or limb numbness. By removing the blockage, atherectomy restores adequate blood supply to the tissues. This improvement translates to a noticeable improvement in the patient's quality of life, allowing for greater physical activity and reduced discomfort. Improved blood flow diminishes the risk of critical events like stroke or heart attack by preventing tissue damage due to oxygen deprivation. This aspect directly impacts the overall well-being of the patient.
- Prevention of Cardiovascular Complications
Restoration of proper blood flow plays a significant role in preventing potential complications arising from arterial stenosis or occlusion. Atherectomy aims to maintain optimal blood flow, minimizing the risk of ischemia in the downstream tissue. By addressing the root cause of the impediment, the procedure can mitigate the risk of future cardiovascular events. This preventative aspect is essential in long-term patient management and underscores the importance of effective blood flow restoration.
- Mechanism of Action and Tissue Perfusion
The improved blood flow is a direct consequence of removing the obstructive plaque. By restoring the lumen of the artery to its original or near-original size, blood flow is facilitated. This improved perfusion provides adequate oxygen and nutrients to the tissues, essential for normal cellular function and reduced ischemic damage. The increased oxygenation of tissues is key in preventing further damage and promoting healthy tissue regeneration.
- Long-Term Benefits and Reduced Risks
Sustained improved blood flow is fundamental to the long-term benefits of hawkone atherectomy. This prevention of re-blockage and maintenance of healthy blood flow reduces the risk of future cardiovascular events. Improved perfusion minimizes the risk of complications, ultimately leading to improved patient outcomes and a better quality of life. The potential for reducing the reliance on medications and improving physical performance further underscores the value of achieving sustained blood flow restoration.
In conclusion, improved blood flow restoration is the primary aim of hawkone atherectomy. The procedure directly addresses the cause of impaired blood flow by removing obstructive plaque. The resulting benefits include reduced symptoms, the prevention of complications, improved tissue perfusion, and long-term enhancement of cardiovascular health. These facets combine to illustrate the crucial link between hawkone atherectomy and the restoration of optimal blood flow for improved patient outcomes.
6. Reduced Recovery Time
Reduced recovery time is a significant advantage associated with hawkone atherectomy. This characteristic contributes to a more favorable patient experience and expedites the return to normal activities. The procedure's minimally invasive nature and targeted approach play a key role in achieving this benefit.
- Minimally Invasive Procedure
Hawkone atherectomy, by its design, involves significantly less tissue trauma compared to traditional open-heart surgeries or extensive vascular interventions. Reduced tissue disruption translates to less bleeding, less inflammation, and a smaller incision site. This minimized invasiveness directly contributes to faster healing and a faster return to normal daily activities. The smaller scale of the procedure often results in a shorter hospital stay and a quicker recovery process for patients compared to more extensive interventions.
- Targeted Plaque Removal
The precise nature of targeted plaque removal facilitates quicker healing. By addressing specific areas of blockage, hawkone atherectomy minimizes the extent of damage to surrounding healthy tissue. The reduced area of impact allows for a more focused healing process. The minimal disruption to surrounding structures contributes to a faster recovery time for patients. This also can lead to reduced pain, discomfort, and the need for extensive post-operative therapies.
- Reduced Need for Post-Operative Intervention
Minimally invasive procedures, such as hawkone atherectomy, often reduce the need for extensive post-operative therapies. This includes fewer pain medications, reduced physical therapy requirements, and quicker resumption of regular activities. Minimizing the extent of the procedure reduces the necessity for extensive follow-up care, contributing to a streamlined recovery process.
- Faster Return to Daily Activities
Reduced recovery time allows patients to resume their daily activities more quickly. This includes work, household chores, and social engagements. A faster recovery enables a quicker return to productivity, both economically and socially. The swiftness of recovery is a key component of the patient experience and contributes significantly to their overall well-being.
In summary, the reduced recovery time associated with hawkone atherectomy stems from its minimally invasive approach, targeted plaque removal, and the reduced need for extensive post-operative therapies. This translates to improved patient satisfaction, a shorter duration of recovery, and a quicker return to a normal lifestyle. This facet underscores the clinical significance of the procedure in terms of patient care and efficiency within the healthcare system. It ultimately contributes to a more favorable patient experience and a positive outcome in terms of their overall well-being.
7. Surgical Precision
Surgical precision is paramount in hawkone atherectomy. The procedure's success hinges on the ability to precisely target and remove plaque from the affected arterial segment while minimizing damage to surrounding healthy tissue. This meticulous approach requires advanced imaging guidance, precise catheter manipulation, and controlled application of the cutting mechanism. Any deviation from ideal precision can lead to complications, such as vessel perforation, embolus formation, or the need for subsequent interventions. The consequence of imprecise maneuvers can range from temporary discomfort to serious long-term complications. Maintaining consistent, high levels of surgical precision is critical for achieving optimal patient outcomes.
The importance of surgical precision extends beyond the immediate procedure itself. Maintaining this standard ensures the preservation of the arterial wall's integrity, limiting the risk of future restenosis. Restenosis is the narrowing or blockage of the artery again after the initial treatment. By minimizing the initial injury and ensuring meticulous removal of plaque, the procedure helps maintain the long-term health of the blood vessel. Examples of such practices in other minimally invasive vascular procedures demonstrate the effectiveness of surgical precision in reducing complications and improving overall patient outcomes. Studies on similar procedures often correlate high precision rates with reduced rates of complications and improved long-term patency of the treated vessel. The significance of surgical precision is readily apparent in these documented instances.
In conclusion, surgical precision is an integral component of hawkone atherectomy, directly influencing the procedure's safety and long-term efficacy. The ability to perform meticulous and targeted plaque removal, with minimal collateral damage, is a key factor in preventing complications and ensuring positive patient outcomes. Maintaining high standards of surgical precision in these procedures is crucial for minimizing risks and maximizing the benefits of this minimally invasive approach to vascular intervention. The clinical implications of this understanding extend beyond the immediate procedure and directly affect a patient's overall long-term cardiovascular health.
Frequently Asked Questions about Hawkone Atherectomy
This section addresses common questions and concerns surrounding the hawkone atherectomy procedure. Thorough understanding of this minimally invasive technique is crucial for informed decision-making. The information provided is intended for general knowledge and does not constitute medical advice. Consult with a healthcare professional for personalized guidance.
Question 1: What is hawkone atherectomy?
Hawkone atherectomy is a specialized technique for removing plaque buildup within blood vessels. It utilizes a catheter with a specialized cutting mechanism to address blockages. This approach is designed to improve blood flow in affected arteries and minimize damage to surrounding tissues. The procedure's efficacy relies on precise targeting of the affected area and the skilled execution of the intervention.
Question 2: Who might benefit from hawkone atherectomy?
Patients with narrowed or obstructed arteries, particularly those leading to the heart or brain, might be candidates for hawkone atherectomy. This minimally invasive procedure is often considered when traditional methods are less effective. The choice of treatment depends on various factors, including the location and extent of the blockage, and the patient's overall health condition.
Question 3: What are the potential risks associated with hawkone atherectomy?
Like any medical procedure, hawkone atherectomy carries potential risks. These include, but are not limited to, bleeding, infection, blood clots, and vessel damage. The risk profile is influenced by individual patient factors and the complexity of the vascular condition being treated. Careful patient assessment and careful procedural execution are critical in mitigating risks.
Question 4: How does hawkone atherectomy compare to other treatment options?
Hawkone atherectomy offers a minimally invasive approach to address arterial blockages. Compared to more extensive surgical procedures, it potentially reduces recovery time and associated complications. However, individual suitability for hawkone atherectomy depends on numerous factors. Consultation with a qualified healthcare professional is necessary to determine the most appropriate treatment strategy.
Question 5: What is the typical recovery process after hawkone atherectomy?
Recovery from hawkone atherectomy generally involves a shorter hospital stay than other types of vascular interventions. Patients typically experience a reduced level of pain, and the recovery period can vary depending on individual circumstances. A healthcare professional can provide guidance on a patient's specific recovery process and expected timeframes.
In summary, hawkone atherectomy offers a specialized approach for addressing arterial blockages. While carrying inherent risks, the procedure aims for precise plaque removal and minimal invasiveness, leading to the potential for accelerated recovery and improved patient outcomes. Thorough discussion with a medical professional is crucial for determining the suitability of this procedure for an individual patient.
The next section will delve deeper into the technical aspects of hawkone atherectomy.
Conclusion
Hawkone atherectomy emerges as a specialized approach to treating arterial blockages. The procedure's minimally invasive nature, coupled with targeted plaque removal and controlled tissue manipulation, offers potential benefits in terms of reduced recovery time and minimized complications. The procedure relies on precise catheter design incorporating advanced imaging and a controlled cutting mechanism. Careful consideration of patient factors and experienced execution are crucial for optimal outcomes. While the procedure presents potential advantages, the efficacy and safety profiles require careful evaluation within the context of individual patient characteristics and ongoing clinical research.
The long-term impact of hawkone atherectomy on patient outcomes, specifically the prevention of recurrent cardiovascular events, remains a significant area for future research. Careful analysis of long-term follow-up data and comparative studies with existing treatments are necessary to fully understand the procedure's place within the broader spectrum of vascular interventions. Continued advancements in catheter technology and procedural techniques will likely refine the procedure, further enhancing its safety and efficacy. Thorough evaluation and clinical studies are critical to solidify its role in the management of arterial blockages.
Paul Maritz: Leadership & Innovation Expert
Hottest Rapper Fortnite Skins
1817 Silver Dollar Value: Price Guide & History